For a person with severe hearing loss due to retro-cochlear hearing impairment, an Auditory Brainstem Implant (ABI) can provide a sense of sound. It is an electronic device that must be surgically implanted. The electrode array is placed on the cochlear nucleus of the brainstem, while another part of the ABI is inserted under the skin.
ABI:s are not as widely used as cochlear implants. By 2010, there were roughly 500 people worldwide who had received ABI:s. In general, speech perception improvements are not as strong with ABI:s as with multichannel cochlear implants.
Background
The ABI was developed in the late 1970s by the neuro-otologist William F. House, in association with the House Ear Institute. The main intended recipient group was individuals with neurofibromatosis type 2 (NF2), a genetic condition that results in benign tumours of the brain, spinal cord and peripheral nerves.
The early version of the ABI included two ball electrodes which were implanted near the surface of the cochlear nucleus on the brainstem. The design evolved over time, and in 1997 an ABI with a 12-electrode array was implanted by Robert Behr at the University of Wurzburg, Germany. This ABI had an audio processor based on the MED-EL C40+ cochlear implant.
Components
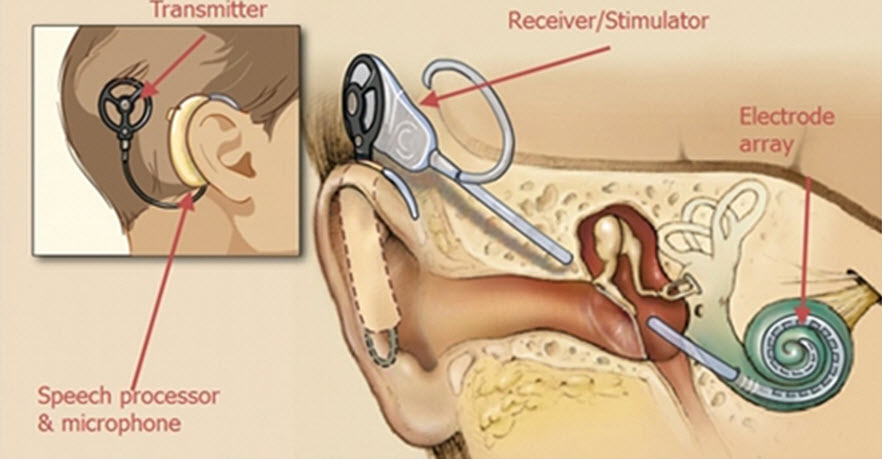
The ABI system consists of two main parts: the external part and the internal part.
External
The external part is worn behind the ear. It contains one or more microphones, the audio processor, and the coil.
The microphones pick up sounds from the environment. The audio processor converts these sounds into digital signals, and send them to the coil. The coil transmits the signals through the skin to the internal part of the ABI system.
Internal
This is the part that is implanted. It receives signals from the coil and send them to the electrode array. The brainstem is stimulated, and this stimulation results the experience of hearing a sound.
While the more famous cochlear implant has a wire-shaped electrode array in the cochlea, the ABI system rely on a paddle-shaped electrode array which is placed on the cochlear nucleus of the brainstem.
Surgery
The surgery required for an auditory brainstem implant is considered more difficult than the one for a cochlear implant, as the former requires a craniotomy (a bone flap of the cranium must be temporarily removed to access the brain). Typically, the surgery requires both a neurosurgeon and a otorhinolaryngology surgeon working together.
During surgery, the ABI electrode array will be inserted through the fourth ventricle and placed onto the surface of the cochlear nucleus.
Patients with neurofibromatosis type 2 (NF2)
If the patient receiving the ABI has NF2, the surgeon will remove acoustic neuroma tumours before inserting the internal part of the ABI. In some cases, the auditory nerve will be removed.
Not only for NF2
Until 2018, ABI was only recommended for patients with the genetic disorder neurofibromatosis Type 2 (NF2). Since then, several countries have also approved ABI for certain other patients who have serious hearing loss but would not benefit from a cochlear implant because their auditory nerves do not function properly. This can for instance be the result of non-NF2 tumours, severe cochlear ossification, and auditory nerve aplasia or hypoplasia.
Outcomes
After receiving an ABI, most patients achieve an improved ability to detect environmental sounds and speech, but the speech perception outcome is typically lower than for the multichannel cochlear implant group.
With an ABI, speech understanding can be expected to improve during the first three years after implantation. Most patients will not reach a level where they can understand speech using only their ABI, but when the ABI is combined with lip-reading skills the outcome is good.
Patients without NF2 generally develop a better speech understanding with their ABI than the NF2 group, and a significant number of them reach a level where they do not require lip-reading to understand speech. It has been suggested that NF2 tumours damage specialized cells important for speech perception.